Abstract
Background: The overall incidence of venous thromboembolism (VTE) has steadily increased in the pediatric population, largely due to rising utilization of central venous catheters (CVCs). Anticoagulation is the mainstay therapy for pediatric CVC-related VTE. Due to paucity of prospective data, optimal duration of anticoagulation therapy has yet to be defined and current recommendations for anticoagulation duration are largely extrapolated from data in adult patients with lower extremity deep vein thrombosis (DVT) and small, non-randomized studies. The objective of this study is to report outcomes of a risk-stratified anticoagulation protocol in a cohort of pediatric patients with CVC-related VTE followed at our center.
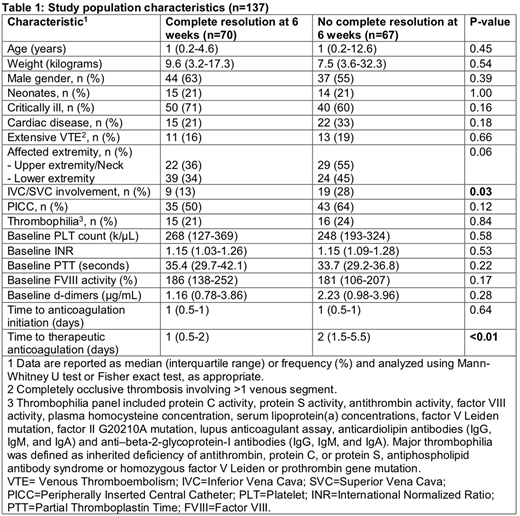
Methods: We performed a retrospective analysis of a prospectively maintained institutional thrombosis patient registry created using Research Electronic Data Capture (REDCap). We identified all patients with an objectively confirmed catheter-related VTE who were followed at our institution over a 5-year period (2012-2017). Patients were managed according to an institutional risk-stratified protocol in which patients received therapeutic enoxaparin for a maximal duration of 3 months with assessment of radiologic response at 6 weeks and 3 months. After 6 weeks of therapy, enoxaparin was discontinued if the CVC had been removed, or decreased to prophylactic dosing if the CVC is still present in low risk patients with non-recurrent CVC-related DVT who had complete radiologic thrombus resolution and no major thrombophilia. We compared patients with complete resolution at 6 weeks to those who did not have complete resolution at 6 weeks with respect to demographics, relevant clinical characteristics, baseline laboratory measurements, anticoagulation quality measurements, and key outcome measures (frequency of a composite of recurrent symptomatic radiologically-confirmed DVT, pulmonary embolism (PE) and/or paradoxical embolism, frequency of post-thrombotic syndrome (PTS), and frequency of anticoagulation-related major bleeding and/or clinically relevant non-major bleeding). Data was compared using the Mann-Whitney U test or Fisher exact test as appropriate. Two-tailed p value less than 0.05 was considered statistically significant.
Results: A total of 137 patients who developed a CVC-related VTE at our institution during the study period were included in the analysis. Of 137 patients, 70 (51%) patients had complete radiologic resolution at 6 weeks, while 26% had partial resolution, 20% had non-resolution and 3% were noted to have radiologic progression. At 3 months, 38% of patients had complete resolution, 24% had partial resolution, 21% had non-resolution and 7% showed radiologic progression. Patients who had complete resolution at 6 weeks were largely similar in their characteristics to those who did not show complete resolution at 6 weeks (Table 1). The frequency of thrombophilia was not different between the two groups and none of the patients were found to have major thrombophilia (Table 1). However, the frequency of vena cava involvement was significantly higher and the time to achieve therapeutic anticoagulation was significantly longer in patients who did not show complete resolution at 6 weeks (Table 1). The frequency of recurrent clinically symptomatic DVT, PE and/or paradoxical embolism in patients with complete radiologic resolution at 6 weeks [5/70 (7%)] was similar to those who did not show complete radiologic resolution at 6 weeks [9/67 (13%)] (p=0.27). The frequency of PTS was significantly higher in patients who did not show complete radiologic resolution at 6 weeks [5/60 (8%)] compared to patients with complete radiologic resolution at 6 weeks [0/64 (0%)] (p=0.02). The frequency of anticoagulation-related bleeding events was similar in patients with complete radiologic resolution at 6 weeks [6/70 (9%)] and patients who did not have complete radiologic resolution at 6 weeks [6/67 (9%)] (p=1.00).
Conclusion: Our study suggests that pediatric patients with CVC-related DVT who demonstrate complete radiologic resolution after 6 weeks of anticoagulation represent a lower risk patient group that appears to have favorable outcomes. Vena cava involvement and longer time to achieve therapeutic anticoagulation may be associated with suboptimal radiologic response at 6 weeks. Larger prospective studies are needed to confirm our results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal